I awoke after my second total knee replacement to learn that all had gone well with the arrival of Mary. That’s the new knee’s name: Mary. George is my first TKR, the left one. Mary is the right. Next would come Bert, my left ankle replacement, followed by Mr. Gower, my right shoulder replacement. And if you’re not a big It’s a Wonderful Life fan, then you should know that George, Mary, Bert, and Mr. Gower are all characters from this classic movie. And with that bit of film trivia, you’ve likely figured out by now that I am a huge fan of the movie (as also evidenced by the title of my first book, Zuzu’s Petals: A True Story of Second Chances). Thus, I have named all my new parts after characters from said movie. Weird, I know, but to each her own, right?
My overnight stay in the hospital was uneventful. I already knew the drill, so nothing was surprising. I ordered the same dish from the kitchen that I had during my previous stay six weeks earlier. I encountered the same routine with visits from the physical therapist, anesthesiologist, surgeon, and physician’s assistant. I even got one of the same terrific nurses from my first joint replacement stay.

I went home the next day with both Jeff and my pal, Liz, who had flown in from California to help. After realizing how hard it was for Jeff to see me in such pain after my first knee replacement, Liz and I had hatched a plan to send Jeff into nature – aka, the closest thing to a church my husband will likely ever set foot in – during the early part of recovery with my second knee replacement. Jeff was thrilled, though he would need to see that I was home and safe before feeling comfortable enough to leave for a few nights. With his backpack loaded in the back of our SUV, Jeff thanked Liz one last time and kissed me goodbye.

Liz cracked a bottle of wine to enjoy while we both dove into the meal that had been delivered that day by one of my local pals. Liz and Clare ate in chairs in my home-office-turned-recovery-room and I stayed in bed, already aware of how tough that first week post-op with a knee replacement can be.
I kept myself as medicated as was allowed, tracking each pill on a chart I kept nearby. Because I had had such a rough experience with my first knee replacement, not to mention that I was still in shock from RuPaul’s accidental electrocution two nights earlier, I had asked my doc if I could take Valium for the first week of recovery, along with all my pain meds, muscle relaxants, and stool softeners. He’d said that would be fine.
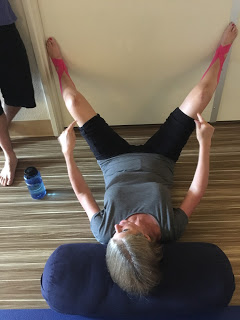
The next morning, I awoke around 7 am, lingering in that middle place between sleep and being fully present, slowly grasping the reality that I now had two new knees, both of which were killing me at the moment. I took my morning meds, hoping I could give them a few minutes to kick in before I wrestled my way up to standing. Using my yoga strap, I maneuvered my first leg to the side of the bed. It was painful; and that was with my older new knee. Oy. Then I lassoed the strap around my second leg, the one with Mary. Got that leg over the edge of the bed and sat resting for a minute. I had pulled my walker in close for the painful process of standing when my body internally screamed at me: I have to pee! Stat!
I was wearing a loose night shirt, T.E.D. compression stockings, no undies. Fourteen feet separated me from the toilet in the next room. Fourteen short feet. Fourteen feet that would’ve been a breeze on any other day, but not necessarily the day after leaving the hospital, the day the nerve block wore off. I struggled to stand in a frantic, herky-jerky manner, gripping the walker as if my life depended on it, willing my bladder to hold on, dear god just hold the hell on!
In great pain and with both Clare and Liz still asleep, I shuffled across the carpet of my office toward the door. Nine more feet to go. Made it to the hardwood floors just outside the bathroom. There was RuPaul, wagging his tail nervously behind the gate Jeff had installed to keep him from coming into my room or bathroom during those first few days. Ru usually slept in our master bedroom upstairs, but with each of my joint replacements, he appointed himself my overnight nurse and would sleep in the closest spot near me, in this case, by the gate that separated us now.
“Sorry, buddy. Gotta pee,” I said, shuffling one foot closer to the bathroom. Four more feet to go.
And that’s when it happened: what I imagine one’s water breaking during pregnancy would be like, had I had a normal pregnancy (hint: I did not). I stood in a puddle of pee, still clutching my walker as the compression stockings soaked up my urine. What was there to do? I wept. Because it all felt like too much at that point. The dog’s near-fatal electrocution two nights earlier, this third of three significant orthopedic surgeries within three months, the pain –Jesus Christ, the pain! And now the pee. If there was ever a “just shoot me” moment during all of my joint replacements, it was then.
I stopped weeping and stared at Ru, now wagging his tail and straining to reach me with his snout over the gate. I shuffled through the other half of Lake Urine and petted my concerned companion, feeling all the worse for having not been there to pick him up at the animal hospital when he was allowed to come home. I knew I couldn’t move the gate because RuPaul would likely track my urine all over the first floor. Plus, there was no one there to control him and sometimes 85 pounds of immature, Great-Dane-sized poodle doesn’t mix well with a couple of brand new knees. And by sometimes I mean always. I had to leave the gate in place.
I slowly turned and shuffled my way back to my bed, pee be damned. I didn’t have the strength to find a towel and throw it on the floor. The mess would have to wait. I grabbed a pair of sweatpants from the stack of clothes on the desk and placed them on the corner of the bed before lowering myself back down on the mattress. There was no way I could reach my feet, let alone pull off a pair of tight, pee-sodden compression stockings, so I put my soggy feet on the sweats and laid back in bed. Then I texted Liz:
Clean-up on aisle five. Sorry, lost all bladder control right outside the bathroom door. Went back to bed. Aren’t you glad you came to be my nurse?
I fell back asleep. It would be a few more hours before Liz awoke. (Fortunately for Clare, she managed to stay in bed even longer, the coolness of her basement bedroom and the lure of summer break allowing for extra-long sleeps.) Without a hint of annoyance or revulsion, Liz cleaned the mess outside the bathroom and peeled the dry but smelly T.E.D. hose off my legs. She could not, however, resist making a few pee jokes at my expense.
I had no more incontinence that day during my trips to the bathroom or to the den to sit in my recliner and watch a movie or chat with Liz and Clare.

At bedtime, I made it through my nighttime routine and again fell into a deep drug-induced sleep, a respite from the constant throb of pain that lay beneath the surface of the woozy daytime opioids. I slept soundly until the early hours of the morning, awaking to take my pain meds before attempting to sit up and move to the bathroom.
Once more, the minute I sat upright, the need to pee urgently demanded my attention. I frantically grabbed my walker and, with great difficulty, made my way to standing before shuffling toward the door. And, once more, guess what happened? You got it. Another clean-up on aisle five. This was no longer mildly funny; it was annoying.
This time, however, Liz was already awake and making coffee in the kitchen. She cleaned up the mess and helped me get into the walk-in shower where I sat on my indispensable shower chair. Let’s face it, by then I was smelling like the New York City subway – in summer – and it was time I attempt my first post-op shower for everyone’s sake.
I handed Liz my nightshirt and in exchange she handed me the box of Glad “Press’n Seal” plastic wrap, which I carefully wound around my new knee to keep the water out. I sat for a long time allowing the warm water to run over my body, long enough that when I was ready to get out of the shower, my feet looked like a pair of purple boots. It was clearly time to elevate my legs, but damn that water felt amazing. With a clean nightshirt and a pair of fresh T.E.D. hose, I sat in my recliner and ate some food that Liz had reheated.
So guess what happened the next morning? Yep, one more clean-up on aisle five. At this point, Liz sent Clare to the store for adult diapers. I think the politically correct term is something like “disposable incontinence pants” and somehow saying that is supposed to help those of us who need disposable incontinence pants retain more dignity. Ha! Listen, once you’ve spent some time in the ICU with everyone and their grandmother poking and prodding and wiping and washing you, the concept of “dignity” seems fairly laughable. I have yet to recover any sense of modesty in front of medical professionals. Not sure if that’s a good thing, but it is what it is.
The following morning, wearing my uber-creepy disposable incontinence pants, I once more made a sprint for the bathroom, “sprint” being a relative term. Yet again, four feet from the toilet my bladder let loose, my pants saturated, urine leaking onto the hardwood floors. Now I had not only a mess on the floor but a mess in my midsection. Liz? Clare? Anyone? Anyone at all?
Later that day, my mother suggested I call the pharmacist and ask him if any of my meds might be causing this new inability of my bladder to keep it together until I made it to the toilet in the morning. I didn’t think much of the suggestion since I had taken all of these medications before without incident. But I called anyway, motivated to get past wetting myself.
“So it only happens first thing in the morning, right?” my pharmacist asked.
“Yep.”
“Tell me what you’re taking at bedtime.”
I listed off my medications.
“Wait,” the pharmacist interrupted. “You said you’re taking a muscle relaxant and a Valium at bedtime?”
“Yep. I still get spasms with my other bad joints and the muscle relaxant seems to help calm my whole body. And the Valium is because the first knee replacement freaked me out so much I asked my surgeon if I could take five milligrams at night. But I’ve taken Valium a few times before so I know my body is okay with it.”
“Lauren, you do know that Valium is also a muscle relaxant, don’t you?”
(Insert sound of crickets here.)
“Um, no. I thought it was to help your brain calm down.”
“Well, your brain is a muscle. And your bladder is too. So you’re basically taking a double dose of muscle relaxants right before you sleep for, what, six hours?”
“Um, yeah.”
(Cartoon lightbulb lights up over my cartoon head.)
“I’d suggest taking one or the other at bedtime, but not both,” he said. Try that for a couple days and see what happens.”
That night, I left the Valium out of my bedtime cocktail. Slept like a log even without it. Awoke in the morning with a full bladder. Relieved myself – not on the hardwood floors, but on the toilet. Remarkable. #idiot
Suffice it to say, I dumped the idea of lowering my stress with Valium. In fact, I dumped the other muscle relaxant as well, realizing that the pain meds alone were enough to allow me to sleep through the deep ache that accompanies the early days of a knee replacement. Lesson learned.
And, thankfully, I haven’t had to put on an embarrassing pair of absorbent paper pants since then.